Yesterday, Representatives Lou Correa (D) and Jack Bergman (R) introduced the Innovative Therapies Centers of Excellence Act (HR 2623). The bipartisan bill—co-sponsored by Reps. Morgan Luttrell (R), Ro Khanna (D), and Dan Crenshaw (R)—would see the VA designate at least five such centres, which would focus on researching and delivering certain psychedelic therapies.
For now, the psychedelics covered by the bill are MDMA, psilocybin, ibogaine, 5-MeO-DMT, and ketamine. Eagle-eyed readers will have noticed Correa’s mention of the bill when we interviewed the pair of politicians earlier this year. But until now, the specifics of the legislative effort have remained a relative mystery.
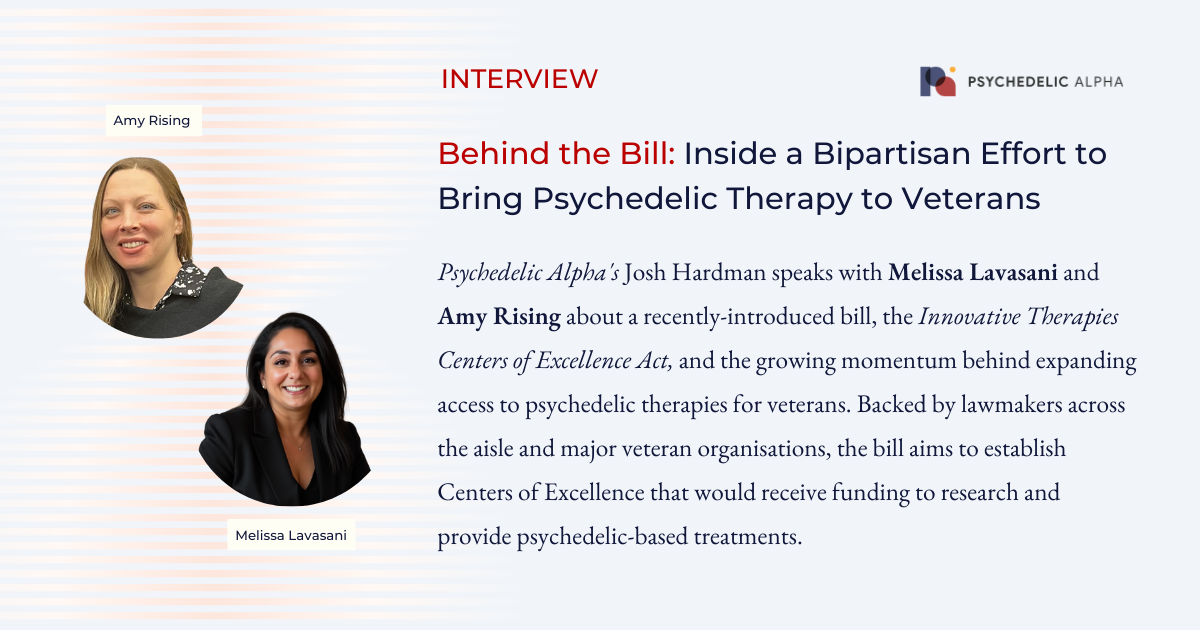
It’s also the first Bill that the Psychedelic Medicine Coalition (PMC) has put its weight behind. The nonprofit, founded by Melissa Lavasani after her own experience with psychedelics in an effort to address postpartum depression, has been pushing for the implementation of psychedelic medicine in the U.S. healthcare system.
The bill itself was largely the product of work by Amy Rising, an Air Force veteran who now acts as an advocate for veterans broadly. With endorsements from across the aisle and support from organisations like the American Legion and the Wounded Warrior Project, the pair hope the bill will become law.
Here, Psychedelic Alpha Editor Josh Hardman speaks with Lavasani and Rising about the bill.
...this is no longer a fringe issue. It’s a serious, cross-cutting policy area with growing recognition on both sides of the aisle that we need to explore new approaches to care, especially for our veterans.
Melissa Lavasani
Josh Hardman, Psychedelic Alpha: From what I understand, this is the first Bill that has received the backing of the Psychedelic Medicine Coalition (PMC). Can you tell us a bit about how this Bill came to be?
Melissa Lavasani: Yes, this is the first piece of Congressional legislation—outside of appropriations requests—that PMC has formally supported. From the beginning, we believed that the first action on psychedelics in Congress needed to come from within—not as an external push from advocates, but as something informed by lawmakers themselves.
Psychedelic medicine intersects with so many different policy areas—healthcare, veterans’ services, research, regulation—that it was important for members of Congress to fully understand the complexities. That’s why the PATH Caucus was created, with its first mission being to “listen and learn.”
Since its formation in November 2022, the caucus has done just that—engaging with the Department of Health and Human Services, the veteran community, researchers, universities, and other key stakeholders. PMC’s vision has always been to assist policymakers in facilitating many of those conversations, helping to ensure that decision-makers had access to balanced, evidence-based information. We’ve been at this for four years behind the scenes to connect dots between science, policy, and patient needs.
The result of all that listening and relationship-building is this bill—truly years in the making. And what’s especially exciting is that it has bipartisan support. That’s a reflection of how the conversation around psychedelic medicine has evolved—this is no longer a fringe issue. It’s a serious, cross-cutting policy area with growing recognition on both sides of the aisle that we need to explore new approaches to care, especially for our veterans.
The timing couldn’t be better—and PMC is proud to support this as a thoughtful, meaningful step forward.
This bill is about holding the VA accountable and ensuring it doesn’t lag behind the science. It’s a chance to bring innovative, potentially life-saving treatments into the fold—because veterans deserve more than the bare minimum. They deserve the best options available, and they deserve them now.
Amy Rising
Hardman: Why is now the time for a Bill like this, with a focus on the VA?
Amy Rising: This is a war of attrition, and right now, we’re losing ground. The rate of accidental deaths—many tied to mental health struggles and substance use—is climbing in the veteran community. The VA’s own data confirms this. That’s not just tragic; it’s a glaring indictment of a system that isn’t meeting the needs of the people it was built to serve. Veterans are slipping through the cracks while relying on a system that too often defaults to outdated or ineffective treatments.
At the same time, we’re seeing federal agencies like the FDA and NIH seriously evaluate psychedelic therapies through rigorous, science-based research. What they have found are evidence-backed approaches showing real promise where conventional care has failed.
This bill is about holding the VA accountable and ensuring it doesn’t lag behind the science. It’s a chance to bring innovative, potentially life-saving treatments into the fold—because veterans deserve more than the bare minimum. They deserve the best options available, and they deserve them now.
Hardman: Can you give us an idea of what the average ‘Innovative Therapies Center of Excellence’ might look like? The bill also envisages those centres having an arrangement with an accredited medical school to provide education and training in these psychedelic therapies. What might those look like?
Lavasani: Each center will likely have its own unique structure and focus, depending on the needs of the region and the capabilities of the host institution. No two will look exactly the same—and that’s by design. We expect there to be a competitive RFP (Request for Proposal) process where VA facilities and medical schools can apply to host these centers. Selections will be based on each institution’s strengths, infrastructure, and experience with innovative or integrative care models.
The collaboration between the VA and the selected medical schools will be critical. These Centers of Excellence won’t just be clinical hubs—they’ll also serve as research and training environments. It’s about weaving psychedelic therapies into the fabric of complex healthcare systems, ensuring both safety and efficacy while building the workforce needed to deliver this care responsibly.
Ultimately, this is about co-creation—bringing together government, academia, and clinical leaders to define what psychedelic medicine looks like in the real world.
The ultimate goal is to make sure veterans can access these therapies close to home, without having to navigate fragmented or overseas care. It’s about turning potential into action.
Amy Rising
Hardman: What does the designation as a Center of Excellence mean in real terms? These centers would presumably be lined up for funding from the appropriations, but what would that be used for? Desk-based studies? Clinical trials? Expanded access? Or, some other access pathway altogether?
Rising: Once designated, these Centers of Excellence would be eligible to receive funding through VA appropriations. That funding is intended to do more than just support research—it would directly enable expanded access to innovative therapies for veterans.
This could include clinical trials conducted within the VA system, along with the development of the infrastructure needed to deliver these therapies on-site. It’s about building out the clinical, administrative, and training frameworks necessary to safely and effectively provide psychedelic treatments stateside—under federal oversight and with qualified medical teams.
The ultimate goal is to make sure veterans can access these therapies close to home, without having to navigate fragmented or overseas care. It’s about turning potential into action.
Hardman: Looking at the list of psychedelics included, do you have a hunch about which might attract the most attention?
Lavasani: While psychedelics are often grouped together, each compound is actually quite distinct in terms of clinical application and therapeutic potential. They’re all on their own trajectory. MDMA and ibogaine, for example, have shown real promise in addressing conditions that are particularly prevalent in the veteran community, like PTSD and mild traumatic brain injury. There’s already a strong foundation there.
Psilocybin is probably the next compound poised for FDA approval, so it’s likely to draw significant attention in the near term. Ketamine is already legally available, but there’s still a lot of work to be done to better understand its long-term safety and how to optimize its use in mental health treatment.
Then there’s 5-MeO-DMT—which could be a bit of a sleeper. It has a very short duration, making it potentially easier to administer in a clinical setting, and its therapeutic potential remains relatively unexplored compared to other compounds.
Ultimately, it’s going to come down to how the VA builds out these Centers of Excellence—how they structure the programs, staff the teams, and match capabilities to the unique strengths of each compound. Every psychedelic listed in the bill, along with any others the Secretary may eventually approve, has a vital role to play in shaping the future of psychedelic medicine within the healthcare system.
Hardman: Is there anything else you would like to add?
Rising: I would like to say also that this a desperate act of love for Jacob David George, Ethan Kreutzer, Matt Kahl and Brandon Ketchum. Four brothers in arms that needed help that wasn’t offered.
Review a copy of the Bill here (PDF).
You might also be interested in our interview with Reps. Bergman and Correa: Forging a Path to Access: Congressmen Correa and Bergman on the Future of Psychedelics in the U.S.