Written by Jeff Fitzgerald and Vicente LLP as part of our Colorado Natural Medicine Health Act Tracker.
Following September’s meeting of the full NMAB the stage was set for the board to officially adopt recommendations in October. That goal proved to be a bit ambitious for some subcommittees with only two groups bringing forth concise recommendations. Administratively, Lorey Bratten is now the full-time director of the Natural Medicine Program. Sam Bahrami, who has been filling in as acting director, has stepped back into his role as Senior Advisor. Mr. Bahrami will continue to play a significant role in the day-to-day management and behind the scenes coordination of NMAB work.
While some aspects of the Natural Medicine program, like cultivation and testing requirements, are more or less settled, the Board is still wrestling with some difficult questions. How many hours of education and supervision should a Facilitator training program require? Who will supervise the first round of trainees? With some board members estimating Facilitator costs reaching as high as $52,500 for the first year of practice for expenses such as liability insurance, facilitator training, product storage, and leasing a space – will the market be large enough to bear the regulations under consideration? The Board is attempting to strike a delicate balance between regulatory safety and program sustainability, a task that may turn out to be the most difficult one of all.
The Emergency Response, Safety, and Ethics subcommittee welcomed several new voices as non-voting participants. Kevin Franciotti, a counselor and drug policy advocate; Kristin Speer, a palliative care pharmacist and co-founder of the Psychedelic Pharmacists Association; and Erica Messinger, a registered nurse and Mushroom Cultivator. Additionally two guest speakers from CDPHE joined for this session. Dr. Steve Cox, the Branch Chief of Home and Communities Facilities and Francile Beights, Policy Advisor at Health Facilities and Emergency Medical Services.
The subcommittee first reviewed the latest updates to Dr. Bradley Conner’s Facilitator Code of Ethics. The maximum number of participants for a group facilitation session, previously capped at 100, was reduced to 64. This number was chosen at the suggestion of Dr. Tina Gonzales to align with the limit on group services that can be reimbursed through Medicaid. Although the possibility of reimbursement for natural medicine services by Medicaid is still unanswered (and debatably never will be answered until we have federal legality), the group chose to align with Medicaid limitations proactively in hopes natural medicine services will be covered in the future. Currently the facilitator:participant ratio is limited to 1:4 in any setting. Other issues discussed included the ability for a participant to decline touch prior to administration, requirements around intake/screening forms, and facilitator consumption of natural medicine while facilitating. Members agreed that screening and intake forms should be standardized by the state. Regarding the prohibition on facilitator consumption of natural medicine, the consensus was that it would be prohibitively difficult to test for or prove. Concerns were raised of the subtle prejudice inherent in allowing pharmaceutical drugs to be consumed by facilitators but not natural medicine. Instead, the subcommittee agreed to utilize broader language such as “a facilitator will not perform natural Medicine Services when impaired” or relying on earlier language stating that a facilitator should “refrain from providing services when personal life prevents them”. Dr. Conner will revise the language for the next meeting. It was also clarified once again that any recommendations made by the NMAB apply only to licensed facilitators practicing in the regulated space. Regardless of the language recommended by the NMAB or adopted by DOR, someone conducting a ceremony under the bona fide exemption would not be expressly prohibited from consuming natural medicine during the ceremony.
Ricardo Baca then reported on the DOR Listening Session on Public Education Campaigns. In that session they discussed successes and failed campaigns from cannabis; the need for clear, plain, unbiased language that appeals to as many people as possible; target audiences including veterans, healthcare providers, community pharmacists, rural community leaders; and effective methods of advertising. The rest of the subcommittee then discussed routes of disseminating knowledge. Suggestions included peer-to-peer education, relying on facilitators and healing centers as knowledge outlets, and engaging respected leaders in rural communities which may not be inherently amenable to natural medicine. Mr. Baca encouraged the subcommittee to move quickly on public education as personal use is already taking place, as well as the need to clearly delineate in the public mind personal use versus regulated access.
The final segment of the meeting consisted of a discussion with Dr. Steve Cox and Francile Bate of CDPHE on At Home Care Facilities. Here the subcommittee was seeking guidance on how to ensure facilitator safety when performing natural medicine services in the home of a participant. Mr. Cox seemed confused at first, appearing to think that the board was thinking at-home facilitation would fall under the purview of the home health care rules. Once it was established that the board was seeking guidance on how CDPHE ensures the safety of home care providers, CDPHE representatives explained the model they use in which CDPHE licenses agencies as entities. Those agencies in turn employ home health providers of varying skill sets. The agency is then responsible for conducting a thorough investigation of the patient and the residence and making a determination on if and how to provide home care. Each home care agency licensed by CDPHE conducts its own version of an investigation. Should Natural Medicine Facilitators need an at home care license before administering natural medicines at a private residence?
Towards the end of the meeting Mr. Cox shared from experience with medical marijuana that any facility that allows Schedule I substances onto its premises is at risk of losing all Medicaid funding. This presents clear problems for hospice and end of life facilities and remains an open question. Hopefully, the state can create a licensing system that is flexible enough to allow separation inside a healthcare facility for natural medicine services.
The next meeting was scheduled for November 8th, 2023 at 1pm.
***
To start off the meeting of Public Health and Health Equity, Sam Bahrami introduced Lorey Bratten, the newly-hired program director for the NMAB. DOR representatives did not attend due to Marijuana Enforcement Division rulemaking. No new non-voting participants were present.
The majority of the meeting consisted of the subcommittee reviewing Billy Wynne’s draft recommendations. These were generally the initiatives the subcommittee has been working on, reformatted into a concise recommendation in a format that the full NMAB could vote on and present to DOR. Recommendations under consideration by the Public Health & Health Equity subcommittee which are highly dependent on the work of other subcommittees were not included. Of nine total recommendations, two were approved for referral to the full NMAB, two were approved for referral to the Products, Research, and Data subcommittee, one was dropped entirely, and four were tabled and will be revisited in the future.
Recommendations approved by motion for referral to the full NMAB:
1. For purposes of the Natural Medicine Access Program, the terms Health Equity and Equity are defined as: Health equity is both an outcome and a process. Health equity happens when everyone has equal and equitable opportunity to be as healthy as they can be. Recognition of one’s race, ethnicity, disability, age, sexual orientation, gender identity, socioeconomic status, geography, or preferred language is vital to promoting equitable health and well-being. Health equity work includes building bridges to positive health outcomes, such as ensuring access to local providers who reflect the diversity of the community that they serve.1
2. The State should establish a clear pathway for Facilitators with Medical or Psychotherapy Facilitator licenses to bill the State Medicaid program for otherwise covered mental health care, substance use disorder intervention services, or behavioral health services that are delivered in conjunction with natural medicine services, in compliance with section 12-179-113(1)(c) of the Natural Medicine Health Act.
Despite existing concerns around facilities that receive federal Medicaid funding potentially losing that funding if they allow Natural Medicine on their premises, this recommendation was approved to encourage the state to begin work on allowing reimbursement for already-covered services.
Recommendations approved for referral to the Products, Research, and Data subcommittee:
1. For purposes of promoting research in and innovation in Natural Medicine as well as reducing the cost of relevant liability insurance, the State should make public all deidentified data collected under the Natural Medicine Access Program. All data must be aggregated to preclude the identification of personal health information.
This recommendation expanded the original suggestion of providing data to insurance underwriters to allow broader public access to anonymized data collected through the regulated natural medicine program.
2. The legislature should clarify the Natural Medicine Health Act to allow Facilitators to purchase Natural Medicine and Natural Medicine Products from Cultivators or Distributors without affiliation with a Healing Center.
Residual questions exist around DEA concerns around storage requirements if facilitators are permitted to remain in possession of Natural Medicine. Rochelle Galey of the BHA suggested looking into the framework of Methadone distribution and storage.
Recommendations tabled pending revision or want of additional information:
1. The State should prioritize accreditation of Facilitator training programs that offer incentives to graduates to commit to offering discounted services to historically underserved or marginalized communities, including those with lower household income, those in rural or frontier areas, those with disabilities. indigenous peoples, racial and ethnic minorities, and those who identified as LGBTQIA+. Such incentives could include discounted tuition or loan forgiveness programs.
Lundy expressed that the better course of action would be to prioritize access to training programs, rather than focusing on who a potential facilitator would be serving. Further discussion elucidated uncertainty around what training programs will actually look like and if the state can partner with existing higher education institutions to expand access. DORA will look into the role of higher education institutions in expanding training program access.
2. The State should include a Health Equity Assessment in the annual report it is required to publish under section 12-179-105(1)(i) of the Natural Medicine Health Act that assesses access to Natural Medicine Services by underserved and marginalized communities, including those with below average household income, those in frontier or rural areas, those with disabilities, indigenous peoples, racial and ethnic minorities, and those who identify as LGBTQIA+.
Although the subcommittee is generally in support of this idea, concerns around increasing costs ultimately resulted in this recommendation being tabled. Changes will likely include language that encourages the state to partner with existing entities that collect this data and placing a theoretical limit of “to the extent possible”.
3. The State should allow licensees to pay licensing fees over a period of months or years, rather than requiring payment in full before the license is awarded.
Issues with this suggestion centered around the fact that the state needs the full license fee up front to fund the operation of the program. DORA staff indicated they will look into options of partnering with a 3rd-party vendor such as Affirm which would allow the state to receive the full fee while allowing a licensee to pay over time. Additional concerns include contracting and procurement processes that could both take a long time to implement and drive up costs.
4. If the legislature authorizes the State to adopt taxation of aspects of the Natural Medicine Program, the State should allocate a portion of those tax revenues to the creation of a Social Equity Licensure Program that offers grants, loans, technical assistance, and other support to individuals and organizations that receive a Facilitator, Healing Centers, Cultivator, Tester, or Distributor license. The State should use clear, enforceable criteria for identifying qualified social equity licensees, such as prior criminal convictions relating to natural medicine or household wealth.
Tristan Watkins of the CBO cautioned the subcommittee not to draw on the cannabis industry heavily given the differences in the sales model and less clear disparate impact of the war on drugs on marginalized communities than existed in cannabis. Combined with the fact that a tax would need to be a ballot measure, the subcommittee concluded this is not feasible by day 1 of the program and will revisit it at a later date.
Recommendations dropped completely:
A requirement that any natural medicine licensee submit a Social Equity Statement indicating their plan to address equity concerns was dropped after discussion elucidated that such requirements are largely ineffective, perceived as virtue-signaling, and seen as unfairly shifting the burden of ensuring equity from the state onto individual businesses.
The next meeting was scheduled for Tuesday, November 14th at 1pm.
***
October saw the addition of one new non-voting participant to the Indigenous and Religious Use and Outreach Subcommittee. Nenette McNamara is a Family Nurse Practitioner and member of the Southern Ute Tribe.
This particular meeting was structured as a review of the work of the other NMAB subcommittees as it affects the Indigenous and Religious Use and Outreach group.
First up was the sphered licensure model under development by the Qualifications, Licensing, and Training subcommittee. Discussion centered on the proposed unified training curriculum and the potential accelerated pathway which would allow for legacy and indigenous healers to become licensed without being required to complete the state-mandated training program. Non-voting participant Sean McAllister, an attorney who works closely with Indigenous groups, suggested allowing for a flexible application that would allow for multiple routes to licensure, such as community signatures as endorsement, rather than focusing on a single test. This idea of licensure through community endorsement resonated with several members. Dr. Sophia Chavez shared that a similar mechanism is used in acupuncture licensure and supported the idea of expanding the options for legacy practitioners to validate their experience and proficiency. She also expressed that the concept of a test is foreign to many indigenous peoples. Mr. McAllister pointed out that most Western-facing retreat centers already take safety seriously (and thus extensive safety training may be unnecessary), that indigenous practitioners generally do not view mental illness as separate from spiritual and relational work, and that the statutory language of SB23-290 permits the board to authorize limited waivers. Subcommittee chair Dr. Pinkola-Estés once again reminded the group of the existing registered psychotherapist model as evidence that the state has the capability to allow the practice of a profession without the need for a state-issued license.
Next the subcommittee reviewed the latest list of potential initiatives from the Public Health & Health Equity subcommittee. Discussion here highlighted the friction between indigenous world views and the world of state regulation. In discussing training program costs, Mr. McAllister again advocated for more flexibility – this time in regards to a sliding scale fee system for licensing indigenous practitioners who may not be able to afford the cost of current training programs. He also pointed out that variation in traditional facilitation practices requires flexibility on the part of the state. Other topics mentioned briefly included benefit sharing arising from the use of natural medicine, the need to bring indigenous perspectives into conversations happening elsewhere in the NMAB, and the need to preserve community and culture in the face of regulation and commercialization by empowering communities. NMAB member Dr. Josh Goodwin, attending as a non-voting guest, shared that work occurring in other subcommittees is lacking an indigenous perspective. In particular questions about facilitator use of natural medicine, outdoor facilitation, and group facilitation as subjects currently under consideration by other subcommittees without indigenous input. Mr. McAllister made an additional suggestion that a facilitator wishing to conduct an administration session that contravenes the established regulations be allowed to request an exception by submitting their facilitation protocol to the state. Senior Advisor Sam Bahrami rounded out the discussion by establishing the state’s need to protect the public. Summarizing this segment of the meeting, Skippy Upton-Mesirow identified a need for more data, suggesting a change in mindset from attempting to define every aspect through regulation to one of “observe and refine”, allowing the program and regulatory scheme to evolve as needed.
The list of draft recommendations from Products, Research, and Data around cultivation and testing was not well received by several members of the subcommittee. They felt that establishing rules governing the cultivation of sacred medicines to be unnatural. Mr. McAllister again suggested that a mechanism allowing traditional practitioners to opt-out of certain aspects of the regulated model could relieve tension in this area. The prohibition on outdoor cultivation in particular drew the ire of the subcommittee. Members shared stories of sacred outdoor sites where mushrooms are grown and emphasized that, for indigenous practitioners, connection to the earth is an integral part of natural medicine practice. Recognizing that there will be practitioners as well as participants who prefer natural medicine cultivated outside of sterile lab conditions, it was suggested that this specific recommendation either have a carveout for indigenous practitioners, or that the state allow for traditionally-cultivated natural medicine, identified with a label or marking describing the techniques with which it was cultivated.
Reviewing the education and curriculum requirements for training programs, Mr. McAllister again emphasized that many spiritual practitioners would opt out of much of the training as not applying to them. A question was raised of how to accommodate healers visiting from other countries, a practice common in the Native American Church. While DORA does have procedures for license portability in many professions, those procedures do not appear viable for accommodating a profession that varies widely and has no equivalent license in other countries. Dr. Josh Goodwin and Veronica Lightning Horse Perez expressed concerns around requirements of continuing education, particularly with regards to uncertainty as to whether the natural medicine market will be large enough to provide the observation hours required under the curriculum. Skippy Upton-Mesirow summarized the final segment of the meeting by identifying three key points:
- Consideration of some form of indigenous/traditional label/stamp for method of cultivation
- In addition to initial facilitator license, elements like ongoing education should have an option to exempt in application
- Bringing indigenous wisdom to recognizing when a facilitator should not facilitate.
The next meeting is scheduled for November 7th at 1pm MT.
***
Several new non-voting participants joined the October meeting of the Products, Research, and Data subcommittee. Dr. Nigam Arora and Dr. Jahan Marcu, a chemist and pharmacologist respectively, are the founders of Marcu & Arora, a consulting firm serving the cannabis and psychedelic markets. Colton Brook, representing the psychedelic testing business Altitude Consulting, was also a new non-voting participant.
Having drafted a list of recommendations for presentation to the full NMAB, chair Dr. Bradley Conner walked the subcommittee through the list, inviting discussion on each recommendation.
The first recommendation called for potency testing of psilocybin and psilocin to be conducted on each “batch”. At the start of the meeting a batch was defined in the draft recommendations as any single flush regardless of size or weight. In a discussion on how to measure and label the potency of psilocybin, Davis Grant of Colorado’s Marijuana Enforcement Division briefly described how psilocybin converts to the active ingredient psilocin and suggested using a formula to determine a “total psilocin content” number. This method mirrors the labeling of cannabis products which include THC-a, THC, and total THC content as separate measurements. The group engaged in a lengthy technical discussion around the necessary number of alkaloids to test for, the fact that psilocybin degrades naturally, and the costs and complications arising from more extensive testing requirements. Heather Krug of CDPHE indicated that the state is likely to require ISO 17025 accreditation for testing labs to ensure consistency in test results across various labs. This generated further discussion on the costs of running an ISO certified lab which served as a segue into discussion of batch requirements and how they relate to testing. Mr. Grant shared how batches and testing works under the MED rules. In that framework the quantity required to undergo testing increases with the quantity of a harvest according to regulations defined by statistically validated methods that ensure a tested sample is representative of the batch as a whole.
The subcommittee spent considerable time discussing how to define a “batch” and a “harvest”. They considered definitions based on weight, harvest date, and quantity of bags or bins. Brian Urankar of the AG’s office advised the subcommittee to craft recommendations in a way that allows flexibility to accommodate future developments in the market. For example, defining a batch by number of bins or bags could proscribe alternative cultivation methods and stifle innovation. Dr. Conner expressed a desire to avoid the problems associated with the 24-hour harvest window that defines a batch in Oregon, leading the conversation to the subject of inoculation. Arriving at the understanding that a single session of inoculation could yield a vast range of batches, the subcommittee differentiated a batch as an inoculation and a flush as the harvest. The conversation concluded with agreement that an inoculation will be used as the baseline definition of a batch, with each flush from that inoculation representing a harvest batch. Each harvest batch would be required to undergo potency testing.
On the subject of species testing, the recommendation of annual, random species tests was generally accepted. The language of the recommendation was modified slightly to allow discretion for the regulator to order remedial measures in the case of a failed species test. A general recommendation to test for microbes and mycotoxins was added, leaving the specifics of those tests to DOR to define in rulemaking.
Regarding the frequency of potency re-testing there was discord amongst the members. Dr. Conner’s initial proposal of re-testing every 3 months received pushback from several non-voting participants who found the 3-month re-testing requirement to be overly aggressive given that, when stored correctly, Psilocybe cubensis can retain potency for up to a year. Those opposed argued that a 3-month re-testing requirement would drive up costs. Recognizing that when a batch would need to be re-tested hinges in part on storage conditions, the subcommittee tentatively compromised on a 9-month retest requirement until stability testing can be conducted to provide a more accurate number.
Next, the subcommittee discussed the recommendation requiring large cultivators to follow USDA MGAP procedures and suggesting them as best practices for small cultivation operations. Finding no real parallel to cannabis with regards to cultivation size, the group considered employee count, output weight, number of bags or bins, volume of fruiting space, and square footage of cultivation area as potential measures of small vs. large growers. The group generally agreed that MGAP standards can impose significant burdens (such as specific facilities requirements) that were undesirable in many circumstances. Given the unlikeliness that a psilocybin cultivator will reach a commercial scale in the first year of the program and the fact that many of the MGAP guidelines around facilities will be covered by other Colorado regulations such as building codes, the recommendation mandating MGAP for large growers was struck altogether. MGAP will be recommended as best practice for all cultivators.
Addressing concerns around diversion of natural medicine products and the need to avoid giving any impression to the federal government that the state is encouraging the production of products that may appeal to children, the example of chocolates was removed from the recommendation that food safety standards be followed when producing any natural medicine product aside from dried or powdered fruiting bodies.
A recommendation that would require all waste products be autoclaved, potentially expensive and unwieldy, was changed to the more general language of “waste should be rendered non-consumable and non-productive for possible further psilocybin production before discarding.”
The next meeting is scheduled for November 15th at 1pm MT.
***
Subcommittee Chair Dr. Alisa Hannum opened the meeting of Qualifications, Licensing, and Training by acknowledging that finalizing the facilitator scope of practice hinges on a deeper understanding of pharmacological and medical contraindications with regards to natural medicine. She updated the subcommittee on changes to the scope of practice since the previous meeting, primarily that the single-license sphere proposed now contains only one “wellness” facilitator license.
To provide the much-needed expertise in pharmacology, the subcommittee heard a presentation from Dr. Ben Malcom, a psychopharmacology expert and consultant. Dr. Malcolm acknowledged that most available clinical trials to date have purposefully screened out any possible contraindications. The resulting dearth of information on interactions and contraindications made it hard to draw bright-line rules regarding psilocybin interactions with other drugs and medical conditions. While there is a small number of medications demonstrated to have acute toxic effects when combined with psilocybin, such as lithium, Dr. Malcolm indicated that most drug interactions exist on a spectrum ranging from slightly diminished effects of psilocybin to increased likelihood of uncomfortable experiences. He recommended that facilitators be trained on identifying possible interactions and implementing a screening process that relieves the facilitator from needing to rely on their own judgment whenever possible.
Next, Tasia Poinsette of the Healing Advocacy Fund presented a study based on interviews with 24 individuals with insight into training requirements, including training program operators, legacy facilitators, and recent graduates of training programs in Oregon. Two takeaways from the report were that many graduates felt underprepared for the work of facilitation following graduation and that direct experience with natural medicine is strongly encouraged. Other suggestions included a more robust practicum requirement, the need for training options that accommodate individuals who already possess significant training in behavioral health, and the need for ongoing interaction with other facilitators in the form of check-ins or peer support groups.
On the subject of training curriculums, the report found a desire for more hands-on training, specifically around dealing with mental illness and trauma. The report generally suggested that certain subjects such as background on health equity and pharmacology are overemphasized in Oregon and could be a smaller portion of the curriculum relative to practical skills of facilitation such as intake and screening practice, de-escalation techniques, and identifying signs of distress, for instance fight or flight responses and dissociation. Several NMAB members and non-voting participants emphasized the need to elevate aspects of the training that focus more on the facilitators themselves through self-care, peer support, and mindfulness skill development. Dr. Sophia Chavez, also on the Indigenous and Religious Use and Outreach subcommittee, felt that these themes were in line with traditional practices which typically see regular check-ins with mentors and ongoing community support. An additional point from the Healing Advocacy Fund report was the suggestion that more responsibility be placed on training programs to vet students to ensure they are in an appropriate place to undertake the path of a facilitator.
Broadly the subcommittee agreed that face-to-face, or at the very least synchronous, interactive online training is far superior to video-based training in this line of work. They also agreed on the value and need for peer-support groups, possibly as a continuing education route. The group wrestled with balancing a demonstrated need for additional hours of training, which would increase costs and decrease access, with the need to adequately prepare potential facilitators for the work ahead. Potential solutions suggested included a stepped form of training, allowing a student to complete some baseline work asynchronously online before moving to an associate-type license that would allow the trainee to be paid while continuing to learn from an experienced facilitator. Dr. Sophia Chavez shared a similar model from her experience studying curanderismo. In that model a student may require up to 2,000 hours of experience before being considered qualified, however those hours could take place outside of a paid training program through working with a master healer.
The subcommittee then moved on to discussing curriculum requirements. Chair Hannum reminded the subcommittee of the statutory requirements to cover certain subjects and identified the two big-picture questions of 1) the hours required and 2) the need to define an accelerated program.
On the draft training requirements, there were minor changes from the previous version, taken from non-voting participant (NVP) James Eshleman. Changes included the addition of an entire module on self-care and a change in the wording of “inner genius” to accommodate the same concept more broadly.
A robust discussion on the format of training followed. The subcommittee and NVP weighed the need for access through online training with the clear need for personal instruction and learning. While no specifics were finalized, the subcommittee generally agreed that a hybrid approach allowing for self-paced, asynchronous training and interactive small-group sessions available online could be a solution. They also agreed that at some point hands-on, in-person training is indispensable to the training process.
Discussing the accelerated option, Ashley Moller of the Attorney General’s office distinguished Oregon, which requires a state-administered exam, from Colorado. The implication being that in Oregon a training program may allow students to opt-out from parts of a curriculum and the state will still verify the required level of competency. This contrasts with the Colorado framework which does not currently allow for a state-administered exam. She cautioned the board to avoid allowing training programs to exempt students from aspects of the curriculum as the state is in essence relying on the training programs to ensure a graduate meets the established competency requirements. Dr. Will Van Derveer described a psychedelic-assisted therapy training program, only open to licensed therapists, that requires 300 hours of training and includes vetting for prior disciplinary action. There was broad agreement that supervised practice and apprenticeship are virtually mandatory to ensure effective training. The subcommittee is still wrestling with who those supervisors will be at the outset of the program. If supervised practice is required to become licensed, who will serve as the first cohort of supervisors? It was suggested by several NVP that volunteering with groups such as Zendo Project could possibly substitute for part of the experimental part of the training. There was also discussion of encouraging new facilitators to work only with smaller doses at first as most information indicated that the most difficult experiences are associated with higher doses.
The meeting wrapped up with the following general agreements:
- Trauma awareness, self-care, and ethics should be emphasized significantly in training
- While there is a need for asynchronous training in the interest of access and equity, that must be balanced with the reality that there is no substitute for in-person, experiential training
- There is a potential problem in requiring supervised hours under a licensed facilitator if there are no licensed facilitators
The next meeting is scheduled for November 16th, 2023 at 9am MT.
***
Finally, the full Natural Medicine Advisory Board convened for updates on October 20th. Sam Bahrami gave his final program update as acting program director at DORA. He shared that in the next week DORA will compile recommendations from all subcommittees for presentation at the full NMAB in November. He will also be reaching out to subcommittee chairs for the purposes of producing a high-level report on the workings of the Board overall. After this update, Mr. Bahrami introduced Lorey Bratten, the new program director for the natural medicine program within DORA. Mr. Bahrami will continue to support the NMAB in his role as Senior Advisor.
For her first public act as program director, Ms. Bratten held a brief election as required by statute for the positions of chair and vice chair of the NMAB. Acting Chair Lundy was unanimously selected to continue in the capacity of Chair while Dr. Bradley Conner was unanimously elected vice chair.
DOR representatives Allison Robinette and Dominique Mendiola then gave an update on the efforts of DOR and the Natural Medicine Division, emphasizing that they intend to continue to support the NMAB in any capacity they are needed. DOR will begin a second round of listening sessions on November 13th, 2023. The next round of sessions will be 2 hours in length and offer an option of in-person attendance. DOR has also opened a full-time position for a Senior Policy Advisor in the Natural Medicine Division.
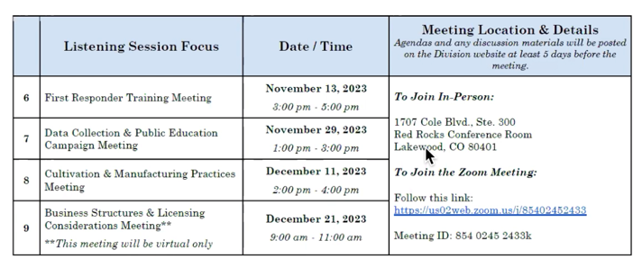
The board then voted to delegate one member to represent the NMAB in each upcoming listening session.
- William Dunn will attend First Responder training
- Brad Conner will attend Data Collection & Public Education
- Sue Sisley will attend Cultivation & Manufacturing,
- Alisa Hannum will attend Business Structures & Licensing Considerations.
Ashley Moller of the Attorney General’s office reminded the board that while the other members may attend and listen to the meeting, any interaction of multiple NMAB members outside of official NMAB meetings could constitute an open meetings law violation.
Moving to subcommittee updates, the first update came from Emergency Response, Safety, and Ethics. The subcommittee reported that they are continuing to refine the Facilitator Code of Ethics, updating the maximum allowable participants in a group to 64, a number chosen at the advice of Dr. Tina Gonzales as a limit set by Medicaid rules. Sam Bahrami briefly discussed the information the subcommittee received from CDPHE regarding regulation of home health care which relies on licensed agencies conducting their own thorough evaluations of patients’ homes prior to providing home health care.
Billy Wynne gave the update for Public Health and Health Equity. Having formulated the work of that subcommittee into recommendations, they have bucketed their recommendations broadly into recommendations they plan to bring to the full board for voting, recommendations that have been tabled pending revisions, and recommendations they intend to convey to other subcommittees as representing the view of the Public Health & Health Equity group.
Following Mr. Wynne’s update, Lundy presented a rough estimate of what potential costs for a facilitator’s license could be. They predict that, in total, a facilitator would need to invest $19,500 by the first day of licensure, including the cost of completing a training program, and that total costs by the end of the first year could be in the neighborhood of $52,500, including the cost of leasing space. This led to a discussion around how sustainable the current framework would be. Dr. Josh Goodwin pointed out that, unlike the usual western mental health model of lengthy relationships with providers, natural medicine participants likely do not represent a recurring source of income. Dr. Alisa Hannum pointed out that high financial pressure could lead to unethical behavior among facilitators.
With the chair of the Indigenous, Religious use and Outreach subcommittee absent, members Dr. Sophia Chavez and Skippy Mesirow gave a joint update. Issues the subcommittee has recognized in the recommendations of other subcommittees include the restrictiveness of a single test-out option in the training program, limitations on group facilitation, cultivation restrictions, and the lack of a mechanism for a facilitator visiting from out of state. Dr. Chavez and Mr. Mesirow shared the subcommittee’s desire for a flexible application that would allow legacy practitioners to avoid the burdens of training through testing out, endorsement of one’s community, proof of experience and work, etc. Other issues raised were the current prohibition on outdoor cultivation and more broadly, that prescribing aspects of natural medicine such as the species used and the cultivation methods run contrary to the indigenous way. Broadly the subcommittee is asking for a framework that is inclusive to legacy practitioners without being overly burdensome and allows both facilitators and the community they serve to thrive spiritually and financially. Dr. Goodwin spoke in support of a more flexible framework and suggested allowing something akin to a label that would indicate natural medicine has been cultivated in a way that follows certain practices that may be important to some communities.
Products, Research, and Data presented their draft recommendations for discussion. Sam Bahrami indicated that the group is still unclear on what level of regulation is appropriate for cultivation. The biggest remaining question outstanding for this subcommittee is understanding the degradation of natural medicine products. This particular puzzle piece directly impacts answers to questions around shelf life, potency, testing and re-testing, and labeling.
Lastly, Dr. Alisa Hannum updated the NMAB on the two big-ticket items the Qualifications, Licensing, and Training subcommittee is working on. The first, Facilitator Scope of Practice, appears close to complete. Following a presentation from a psychopharmacologist in October’s subcommittee meeting, Dr. Hannum will make minor adjustments to the scope of practice to reflect specific safety concerns. Speaking about the training and education requirements, Dr. Hannum felt the subcommittee has significant work to do in that area. The information the subcommittee received from both non-voting participants as well as a study from the Healing Advocacy Fund indicated that the training requirements in Oregon are inadequate in certain aspects. Currently the subcommittee is faced with something of a chicken and egg problem – to require new facilitators engage in supervised or observational work under trained facilitators, you need facilitators. Regarding an accelerated training option, the subcommittee will focus on a flexible application to bypass some or all of the training requirements.
At the close of the meeting NMAB chair Lundy reminded members that the bylaws prohibit missing three consecutive meetings or 5 meetings total in a calendar year. They also requested that each subcommittee prepare finalized recommendations in a form that the NMAB can vote on for the next meeting.
The next meeting was set for November 17th, 2023 at 1pm. The program director will also share the full schedule of 2024 meeting dates in the next meeting.
Weekly Bulletins
Join our newsletter to have our Weekly Bulletin delivered to your inbox every Friday evening. We summarise the week’s most important developments and share our Weekend Reading suggestions.



