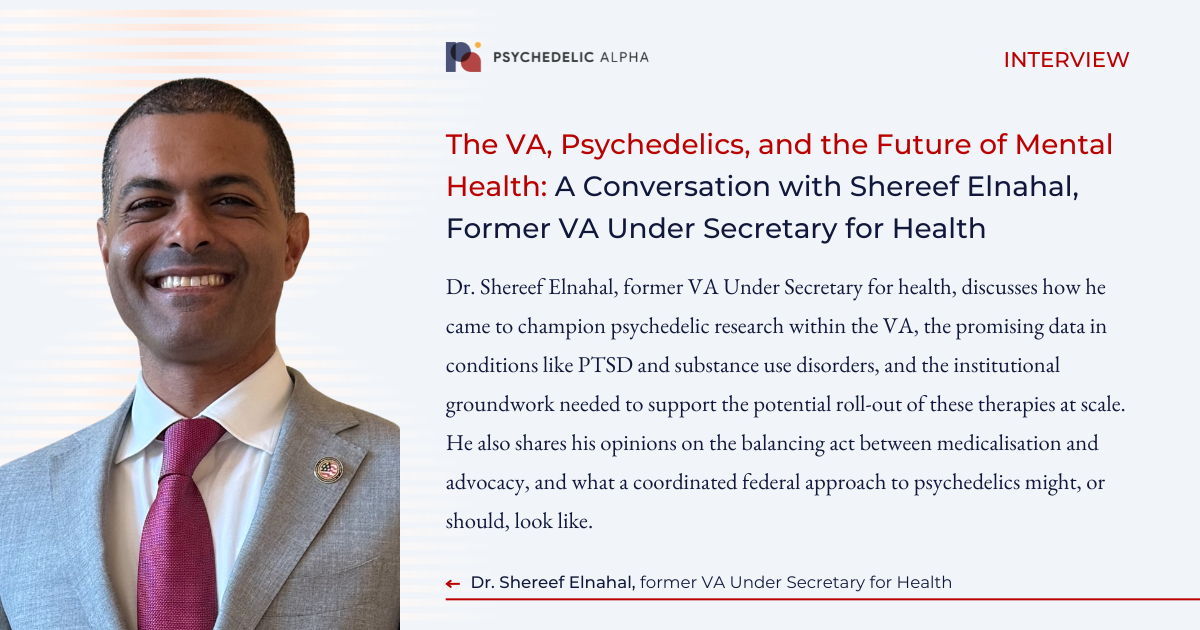
Dr. Shereef Elnahal has spent much of his career at the intersection of medicine, policy, and public service. As the former Under Secretary for Health at the U.S. Department of Veterans Affairs (VA), he oversaw the nation’s largest integrated healthcare system. Through that role, he learned that a growing number of veterans are exploring the potential of psychedelic-assisted therapy to address high rates of conditions like PTSD, depression, and traumatic brain injury.
Elnahal soon became known as something of a psychedelics champion within the VA, pushing for greater research and roll-out preparedness activities. Last May, he told an audience at Horizons’ 16th conference in New York City that he believed demand for MDMA-assisted therapy would “go through the roof”, if approved. Despite the lack of an approval, the VA ploughed forward with its psychedelics research agenda, with Elnahal expressing an openness to working with industry during his time at the agency.
On a sunny afternoon in Berkeley, California, Psychedelic Alpha Editor Josh Hardman caught up with Elnahal, who is now something of a free agent, aside from a gig as Executive Health Advisor with Thrive Capital.
In this interview, Elnahal discusses how he came to champion psychedelic research within the VA, the promising data in conditions like PTSD and substance use disorders, and the institutional groundwork that has been, or is to be, laid to support the potential roll-out of these therapies at scale. He also shares his opinion on the balancing act between medicalisation and advocacy, and why he believes a sort of professionalisation is key to winning support from key stakeholders in the prevailing medical establishment. Finally, he offers insight into what a coordinated federal approach to psychedelics might, or should, look like.
...the memories are so painful for so many veterans that they can't complete these therapies, and so they have sought out alternatives, mostly for that reason.
Josh Hardman, Psychedelic Alpha: How did you first come across psychedelics?
Shereef Elnahal: It was through my work at the VA. I met a number of veterans in the field, visiting medical centers and clinics, and whenever I did so, just to get to know my teams better and understand local priorities throughout the 50 states and territories where we had infrastructure, I would always try to do veteran roundtables to understand the direct perspective of our customer and to get a better sense for what we could do to meet their needs.
Invariably, we would see veterans with mental health issues across the spectrum, including PTSD and treatment-resistant depression, and a number of them had gone through experiences, most through underground and unofficial channels, domestically and abroad, with psychedelics to address their mental health conditions. I heard these stories over and over again in my travels.
I then came to discover that I had entrepreneurial leaders in the VA who had been facilitating studies on psychedelic-assisted therapy with MDMA and psilocybin for a number of years. So, I brought them in to understand what they were doing and how they were doing it.
It was interesting, because this work was a bit underground, even at their level, with previous leadership in the agency. There was this situation where veterans themselves were telling me about the importance and promise of this and senior leadership and mental health, including Dr Ilse Wiechers and others, were actually helping to build the evidence base behind it.
So I said: Why aren’t we doing more of this? Why aren’t we starting to fund some of these studies with our research dollars appropriated to us every year? And why aren’t we engaging the broader community invested in looking closely into the efficacy and safety of these therapies?
Instead of asking the question, I pursued it and decided to take ownership of what could be a really important revolution for veteran mental healthcare.
Hardman: And what other things were coming up at these roundtables you held with veterans? I know Congressman Lou Correa has been hearing from veterans that they’re interested in cannabis, for example. What about other interventional psychiatry treatments, like TMS? Though I understand for PTSD there is not an enormous field of options.
Elnahal: You have a standard of care set that includes prolonged exposure therapy, SSRIs, cognitive processing therapy. These work if the patient is able to go through and complete the treatments reasonably well, which is why we still advocated for the evidence based therapies that existed.
But what makes these conditions unique in veterans is how they are tied to traumatic memories that are just debilitating in the process of recalling them, and the entire idea behind a lot of these therapies is to desensitize your reaction to these traumatic memories so that you can function. But the memories are so painful for so many veterans that they can’t complete these therapies, and so they have sought out alternatives, mostly for that reason.
The fact that they’ve had to go abroad to seek those alternatives, in therapeutic environments where we had no line of sight out of the VA or any of the regulatory bodies of government, meant that that we couldn’t ensure their safety. So, for a very practical reason, getting the full medicalization and professionalization of psychedelics, and surfacing the evidence behind what these agents can do with their risks, just makes for a much safer and better environment for treatment overall.
What’s striking about the early data we have on these agents is how profound the effect size is. No therapy works for 100% of patients, and it's very rare that the therapy is so definitive and curative for these really tough conditions, but the results are still impressive.
Hardman: I think many people would agree that it seems wrong for veterans to be going to receive psychedelic therapy somewhere where you have no oversight, having to do all of this out of pocket, abroad. I think there’s a lot of bipartisan consensus there.
So what exactly did your work look like in the VA, in setting up the studies, the integrated program team, and so on?
Elnahal: What’s striking about the early data we have on these agents is how profound the effect size is. No therapy works for 100% of patients, and it’s very rare that the therapy is so definitive and curative for these really tough conditions, but the results are still impressive.
The MAPS/Lykos trials showed very high rates of loss of PTSD diagnosis and full remission from PTSD symptoms. The Bronx VA was able to replicate those results, with really important work that Dr Rachel Yehuda did in veterans. So we knew that the results were not only reproducible, but reproducible in veterans. The same goes for the investigations we were doing on psilocybin, again, all supported by external, mostly philanthropic, funding sources. We were seeing some of these really promising effect sizes in the veteran population, and we were also very careful about documenting risks and adverse events where they happened.
It turns out the safety profile in these control trials is quite good. You have to be careful about the way you conduct these trials, especially the process of weaning veterans off of their normal treatment regimens such as SSRIs; that can be the most risk prone aspect of these interventions. But if you do this in a supervised way, the supportive way for patients, the potential is certainly there.
This really compelled us to get the expertise of all of the clinician scientists in the VA doing work on psychedelics, not just in the clinical trial realm, but also upstream in basic science and translational research, into a single meeting that we called the Psychedelic State of the Art Conference in Colorado. I remember attending this and the full readout of all the breakout groups, the different sort of phases of research, and I just learned a ton from the expertise from these folks.
For the first time, there was a process by which the VA could prioritize its approach to this, and we ended up publishing that.
I think that was a really important foundational step, because it informed what we were prioritizing on behalf of veterans. It also built relationships for collaborative work, which is a very practical outcome, and created the foundation for understanding what priorities need to be funded. Then we started using appropriated research dollars for the first time to fund these studies.
I was only there long enough to fund the very first multi-site trial that came from this effort. It was a trial that looked at MDMA-assisted psychotherapy in veterans with concomitant PTSD and alcohol use disorder, which is very common in veterans with PTSD. The scientific community hasn’t proven the case in large cohorts of people who simultaneously had another substance use issue, and there are interesting hypotheses about simultaneous treatment of multiple behavioral health conditions with these agents. So the endpoints of that study won’t just be around loss of PTSD diagnosis and remission from PTSD; it’ll also be around what that journey is with alcohol use disorder.
We were prepared to fully scale and implement as many sites as possible to deliver MDMA-assisted psychotherapy should the FDA have come to a different decision than they did. My fear at that time was being in a situation where we didn't have the infrastructure or the investment or the preparation to scale MDMA.
Hardman: That’s interesting. People in the field often talk about psychedelics as having transdiagnostic potential, being something of a blunt instrument in many mental health conditions. That might also get at the point that the lines between mental health disorders are more blurred than the DSM lets on. But it’s difficult, at least in the drug development model of clinical research, to study multiple indications in one study.
I guess groups like VA and more academic sites have this opportunity to do this type of work, though, which a lot of people are very excited about.
Elnahal: Yes, and the VA has probably the best infrastructure for large, multi-site mental health trials, mostly because of the world class personnel. We have some of the best clinician scientists in mental health, because that’s what veterans need in our system, but we also have the scale and resources to be able to do good work, and so putting those resources to bear on psychedelics is really important.
I think the agency is going to fund more studies with these research dollars, and it’s exciting to see that psilocybin will be included, and more collaborative work will be happening with companies doing clinical trials with submissions to the FDA for possible approval. Some of those sites are going to be in VA medical centers serving veterans, and so they’re going to be developing unique insights as well.
Hardman: So the sponsor will still be funding it, but they might be using VA sites?
Elnahal: Exactly. Usona is one company that had some sponsorship of VA sites as trial sites. It will be really interesting to see that VA is contributing to that eventual assessment from the FDA.
Hardman: Interesting. You mentioned Ilse Wiechers earlier, who worked closely on the esketamine IPT. How many of the learnings from esketamine’s VA rollout, which was catalyzed by the first Trump administration, are going to inform what happens with psychedelics?
Elnahal: We were prepared to fully scale and implement as many sites as possible to deliver MDMA-assisted psychotherapy should the FDA have come to a different decision than they did. My fear at that time was being in a situation where we didn’t have the infrastructure or the investment or the preparation to scale MDMA. So, starting about a year in advance, Dr. Wiechers, having the foresight that she does, started preparing our medical centers that were already engaging in research to be able to quickly translate that into frontline clinical care with MDMA. So we had dozens of sites prepared to do this, and my fear was that it still wouldn’t have been enough to meet the surge in demand that we would have expected.
That kind of experience would have been seen across the country for people demanding MDMA assisted therapy because of how operationally intensive that therapy is. So, one silver lining of the FDA coming to the decision that it did is that we have the time to explore different treatment models and modalities. What does it look like when you combine MDMA with prolonged exposure therapy? Can you do that in a shorter course of therapy? There are some really promising results, preliminarily, coming out of some groups looking at these questions, including whether you can do psychedelic assisted therapy in group settings, or whether you can reduce the number of MDMA sessions and overall numbers of therapeutic sessions to get to a more efficient delivery system.
These are really practical questions that will be important for scaling access to therapy by simply creating more slots for veterans and patients, more generally, to get it. We need to be taking advantage of this time, this delay, because I do think MDMA and psilocybin will be FDA approved at some point. Taking this time to test more scalable, operationally efficient models to deliver therapy will make that access more equitable.
I think it's incumbent upon everybody who is trying to medicalize and professionalize this to use the channels that already have at least some degree of trust. I know that trust in institutions, more generally, is compromised right now, but they still hold a lot of weight with the bodies that will absolutely be needed.
Hardman: You have left your role at the VA, and I think you know some in the psychedelic field were upset by that news because you were seen as something of a champion for it.
Let’s imagine for a moment that you are now appointed to run a task force on psychedelic research and implementation, either in the VA or more broadly. What would your agenda be? How would you be going about it?
Elnahal: Look, I will always consider opportunities to serve the country, I’ve done that my whole career. When you leave government, the very next day you are definitionally no longer current, so I’ll start my answer by saying that not being in the arena right now limits my insights into what we should do, because those insights are always richer when you’re in it.
I do think the promise of psychedelic assisted therapy for mental health, based on the data, the effect sizes and the stories I’ve heard from veterans, would benefit from a government-wide approach that was centrally coordinated by the White House or by HHS, bringing agencies together to meet multiple parallel goals.
There are a substantial number of things that the federal government needs to do to actually get us to the end point of equitable access to these therapies. For example, the DEA needs to assess whether rescheduling these drugs right now is a good idea. I would advocate, based on the evidence that does exist, that they should not be schedule one: there are clear medical and therapeutic benefits in certain contexts with these agents, so I don’t think they should be classified as schedule one.
That’s also necessary for actionable work that would happen after FDA approval, which is entirely based on the trial results submitted in the multiple phases and the FDA’s assessment of benefit versus risk. But ultimately, the FDA advisory committee that assessed the first round of the MAPS/Lykos trials weren’t just cognizant of the data and the outcomes, they were cognizant of the potential implications of blessing the first approval of a psychedelic agent for medical use.
That, I think, layers on a different set of challenges. We need to start embedding this type of work more meaningfully into the trusted institutions of medical research, and that means the professional societies. It means getting more powerhouse academic centers like Hopkins and Wash U to hire faculty who have experience in this and start centers of excellence, like the one that exists already at Hopkins. You need to also make sure that entities like the American Psychiatric and Psychological Association, American Medical Association, and other groups that broadly represent the mental health community start thinking about how to emphasize this work in their own infrastructure. Do they have their own centers that look at this critically? Are the people interested in this competing for board seats and leadership positions?
I think it’s incumbent upon everybody who is trying to medicalize and professionalize this to use the channels that already have at least some degree of trust. I know that trust in institutions, more generally, is compromised right now, but they still hold a lot of weight with the bodies that will absolutely be needed. That includes the advisory committees to the FDA, the Drug Enforcement Administration, senior leadership now at the VA and Health and Human Services, leadership at SAMHSA and these institutional players. The movement needs to co-opt the structures of long standing institutions in American medicine.
The other thing I would say is there needs to be a clearer and crisper separation between folks studying these agents for medical use and advocates who are looking for reform at the state level or otherwise on safe adult use. I think in the infancy of psychedelics being investigated for medical purposes, the stigma created by the war on drugs and more generally by our culture didn’t allow for the luxury of advocates to not be involved. Advocates needed to be involved because they were the most bold at that point. But now there are enough folks who grew up in completely different environments, went through formal medical and scientific training, and have august research portfolios in other spheres of mental health who see the promise in this. We’re at a different stage now where organizationally, but also person by person, we need to decide who’s doing what, and we need to put a lot more rigor and seriousness behind medical research.
I think we benefit now from the sheer number of professional scientists doing this work. We should support them by making those lines clear that will allow for the milieu for FDA approval and everything that comes after.
Veterans have asked me questions like: ‘Is the VA listening to us? So many of my battle buddies and so many of my friends who I served with have changed their lives for the better, but some have gotten hurt.’ Elucidating how to maximize the people getting better and minimize the people getting hurt requires us to advance that research.
Hardman: It’s a sensitive subject, the ‘professionalisation’ or medicalisation of the field, with some people that have been working on and with psychedelics for a great deal of time expressing discomfort around it. There’s a common refrain among some psychedelics advocates that goes something like: ‘We should not make psychedelics mainstream, we should make the mainstream psychedelic!’
Elnahal: Well, this is not to say that there isn’t a ton to learn from traditional settings where these therapies have been administered for centuries. That experience is valuable, and if you look at how these protocols are administered, there are very intentional steps around integration after psychedelic experiences that allow for the period of time where you’ve got neuroplasticity happening and you’re truly in a stage where you can change for the better and you can overcome your trauma. The cultures that have been administering this for centuries understood that and have embedded it in their traditions.
But we also have to work within a system that is responsible for the safety of the American public, and that means generating the most robust data possible and putting the best and most serious players behind the research producing that data.
Hardman: So now that you have left the VA, how are you planning to continue being involved in the psychedelics field in this effort, if at all?
Elnahal: From the standpoint of trying to advise on federal policy to generate more and better data on safety and efficacy and risks, I stand ready to help organizations inside and outside of government on how to think about that. I have gone through the process of getting consensus within federal agencies to do more of this work, speaking the language of members of Congress who hear from constituents about this every day.
Some of the best allies that we had for the research we were doing were people like Congressman Morgan Luttrell, a Texas Navy Seal who very publicly tells his story about going through a psychedelic experience to help his mental health, people like General Jack Bergman, who represents the Upper Peninsula of Michigan, knowing and seeing folks that he may have mentored his whole career go through this and come out for the better. Those kinds of allies in a bipartisan way are absolutely needed to respond advance this work responsibly, and I think that’s what veterans are looking for. They’ve told me that directly, and I do think this field of work will be very important in determining the degree to which veterans trust the VA into the future.
The question of whether VA is leading on this type of research is a larger question than just that. Veterans have asked me questions like: ‘Is the VA listening to us? So many of my battle buddies and so many of my friends who I served with have changed their lives for the better, but some have gotten hurt.’ Elucidating how to maximize the people getting better and minimize the people getting hurt requires us to advance that research. ∎